How to Interpret CGM Data for Optimal Health and Athletic Performance

🎧 On the go? Listen to this episode on The GOOD IDEA Audio Blog, available on Spotify or Apple Podcasts.
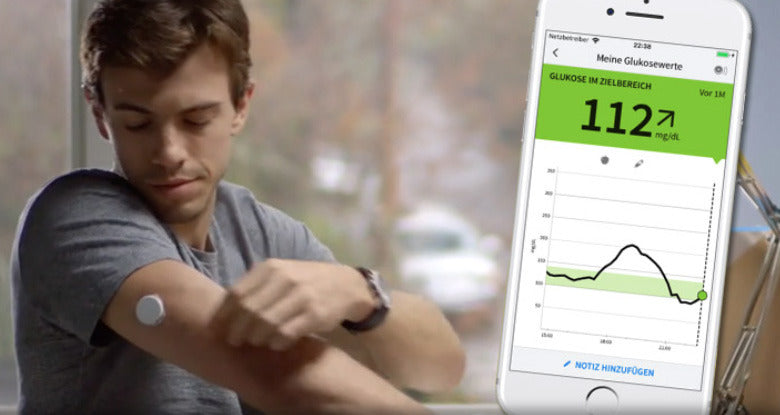
Continuous Glucose Monitors (CGMs) were first developed as a way to provide a real-time measure of blood sugar levels to help individuals monitor their diabetes. However, in recent years, they have revolutionized the way non-diabetics monitor glucose levels, providing actionable data that can be invaluable for optimizing health and performance. Health tools like CGMs can provide incredibly helpful data, but this information is only useful if we know how to interpret the information we receive. This interpretation isn’t always straightforward as it will vary based on individual goal goals, health status, and daily activities. So, we are on a mission to help make CGM interpretations more straightforward by providing basic guidelines based upon your goals. Keep reading to discover the basics of reading and interpreting CGM data to help you make informed decisions about your health and well-being.
Understanding CGM Data

A CGM measures glucose levels in the interstitial fluid, providing continuous updates throughout the day. This data is displayed on a graph, with time on the x-axis (horizontal axis) and glucose levels on the y-axis (vertical axis). Before diving into interpretation, it's essential to understand key terms:
- Glucose Levels: The numerical value indicating your current glucose concentration, typically measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L).
- Trend Arrows: Arrows pointing up, down, or sideways indicate the direction and rate of change in glucose levels.
- Time in Range (TIR): The percentage of time spent within a target glucose range. For most CGMs you can set a custom range, however the default is usually between 70-180 mg/dL or 3.9-10 mmol/L.
One of the challenges of interpreting CGMs is that they were originally developed for people with diabetes. It wasn’t until recent years that they started to be used as a proactive way of measuring our health status. Thus, we have very few scientific studies that incorporate glucose numbers for healthy individuals. This means we do not have solid cut-off values for what is healthy following certain activities. Adding to the complexity, our blood sugar changes based on sleep, food choices, health status, activity levels, and many more factors. This makes establishing normative values challenging.
However, there are general principles that can be applied to not only understand our data but act upon this information to improve our health.
Interpreting CGM Data for Health Optimization
- Baseline Glucose Levels: Start by understanding your typical glucose range during fasting or non-meal times. The easiest way to do this is to take note of your blood sugar immediately upon waking as well as what your blood sugar seems to level off at between meals. This baseline helps identify deviations and patterns.
- Meal Impact: The foods we eat play an extremely large role in our blood sugar levels. Take note how meals affect your glucose. Foods that contain a high amount of simple sugars, like candy, sugary sodas, or heavily processed foods, significantly spike blood sugar levels. On the other hand, lean proteins, healthy fats, fiber, and functional beverages (like GOOD IDEA) help to stabilize blood sugar levels. Some foods (like oats and bananas) have an individualized response so it’s best to test these foods for yourself with a CGM. In order to optimize metabolic health, focus on foods that stabilize blood sugar. Try to avoid sudden post-meal spikes and the dramatic dives in blood sugar that follow. Track how long it takes for glucose levels to return to baseline (shoot for a return to pre-meal glucose levels within two hours for individuals that are metabolically healthy).
- Exercise Response: Monitor glucose trends during and after exercise. Some people experience glucose drops (hypoglycemia) or rises (hyperglycemia) depending on exercise intensity and duration. Rises in blood sugar during exercise are perfectly normal. It is your body’s way of mobilizing the energy you need to fuel your activity. A dip in blood sugar during extended high intensity exercise can indicate that you may have utilized your circulating and stored glucose (aka glycogen). In this case, a snack containing carbohydrates can help to bring glucose levels back to normal levels.
- Stress and Sleep: Consider how stress and sleep impact glucose levels. Stress can elevate glucose, while poor sleep may lead to higher fasting levels and impaired glucose metabolism throughout the day. If you are experiencing glucose levels that are higher than normal after a night of poor sleep, try performing some high-intensity interval exercise. Research has shown that high-intensity exercise can help to reduce the negative effects of impaired sleep.
- Pattern Recognition: Look for recurring patterns, such as morning highs (dawn phenomenon) or nighttime lows (nocturnal hypoglycemia). Adjust lifestyle factors accordingly. If you see patterns that you are unsure of (like consistently elevated blood sugar or glucose that is abnormally high upon waking) then be sure to consult with your healthcare provider.
Using CGM Data for Performance Optimization

- Pre-Exercise Planning: Check glucose levels before exercise to ensure they are within a safe range. Adjust carbohydrate intake if needed to prevent hypoglycemia or hyperglycemia during workouts. If you are about to perform low-intensity exercise (like walking, jogging, casual bike riding, or pickleball) then pre-workout fueling is likely unnecessary since these types of exercise predominantly rely on our endogenous fat as fuel. If high-intensity exercise is on the schedule then monitor your CGM to be sure that your glucose trend arrow is not steeply increasing or trending down immediately before exercise.
- Intra-Exercise Monitoring: Monitor glucose trends during prolonged exercise sessions. A rise in blood sugar at the beginning of exercise is completely normal and can be helpful to power your workout. Watch for a trend arrow pointing down or glucose levels dipping below normal, this indicates that you are utilizing your existing blood sugar to fuel your exercise. In this case, consuming carbohydrates can help to prevent crashes (aka “hitting the wall” or “bonking”) and maintain a high-intensity workout. For our complete guide to sustained energy levels read our blog “How to Control Blood Sugar to Fuel Your Workout.”
- Post-Exercise Recovery: Analyze how glucose levels respond post-exercise. Focus on refueling with a balanced meal or snack to support recovery and glycogen replenishment. Try to refuel with protein and carbohydrates (the ratio of protein:carbs will be dependent upon your exercise and your performance goals). If you are curious about what refueling plan will help you to optimize your goals then check out or blog on post-workout fueling.
- Hydration and Electrolytes: Consider the impact of hydration and electrolyte balance on glucose levels, especially during endurance activities.
- Long-Term Trends: Review trends over time to identify areas for improvement. Work with a healthcare professional or nutritionist to optimize nutrition and lifestyle choices for better performance outcomes.
CGM Takeaways
Continuous glucose monitoring provides valuable insights into glucose dynamics, allowing for personalized optimization of health and performance. By learning to interpret CGM data effectively and making targeted adjustments, individuals can achieve better glucose control, enhance athletic performance, and promote overall well-being.
Author: Dr. Colleen Gulick
*This blog is not intended as medical advice. Please utilize CGM data as a tool for continuous improvement and work collaboratively with healthcare professionals to develop tailored strategies for your unique needs.